Osteochondrosis of the thoracic spine is a degenerative-dystrophic chronic process of damage to the intervertebral discs and vertebral bodies of the thoracic spine. This disease is somewhat less common than osteochondrosis of the cervical or lumbosacral spine. However, this does not mean that it does not cause the person any problems. Osteochondrosis of the thoracic spine mainly manifests itself in back and chest pain, but it can also cause pain in the heart and abdomen, similar to angina pectoris or hepatic colic. In rare cases, osteochondrosis of the thoracic spine becomes the cause of the development of paresis of the muscles of the lower extremities, impaired sensitivity in them and disorders of the pelvic organs. Treatment of the disease consists in the use of drugs, and non-drug methods, and sometimes even surgical intervention is required. In this article, you will learn about the symptoms of thoracic osteochondrosis and its methods of treatment.
thoracic spine
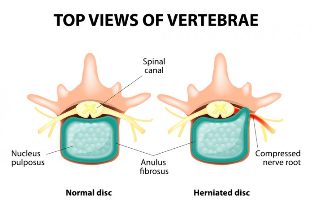
The thoracic spine is represented by 12 vertebrae with intervertebral discs between their bodies. The discs consist of a nucleus pulposus and an annulus fibrosus. Pathological changes in these intervertebral discs, as well as in the adjacent facet joints, the growth of bone spines along the edges of the vertebral bodies, dystrophic processes in the ligaments of the spine and the direct cause of back pain.
It goes without saying that osteochondrosis as a disease rarely affects only part of the spine. Usually this process is diffuse and more or less pronounced in different parts of the spine.
Some structural features of the thoracic spine mean that it is less likely to be affected by osteochondrosis than other regions of the spine. Let's list these features:
- less mobility of the thoracic spine;
- the presence of points of connection of the vertebrae with the ribs (which, when combined with the sternum, form a strong frame of the chest, less prone to injury);
- low thickness of the intervertebral discs;
- physiological kyphosis (curve in anteroposterior direction with a backward bulge) of the thoracic spine, and therefore the maximum axial load falls on the anterior rather than the posterior parts of the intervertebral discs.
Another feature not of the structure, but of the development of osteochondrosis of the thoracic spine, which also determines the lower frequency of pain in the thoracic spine, is that the existing morphological basis of osteochondrosis in this part for a long time clinically "stupid"can stay. That is, there are changes, but they do not bother the patient.
And yet, with provocative factors such as a sedentary lifestyle (including years of working at a desk or driving a car), injuries, poor posture, sagging back muscles, hard physical labor in a forced position, osteochondrosis of the thoracic spine shows its real face.
Symptoms of osteochondrosis of the thoracic spine
The main clinical symptom of osteochondrosis of the thoracic spine and other parts of it is pain. Back pain, chest pain, even pain in the internal organs. In medicine, it is customary to distinguish several pain syndromes (and not just pain syndromes) of osteochondrosis of the thoracic spine. Overall, they are divided into two groups:
- reflex;
- compression.
Reflex syndromes are clinical manifestations of stimulation of the spinal receptor. These are receptors for ligaments, capsules of intervertebral joints, intervertebral discs, which receive pathological impulses in osteochondrosis. In addition to pain, reflex syndromes can also be accompanied by muscle tension, vegetative disorders in soft tissues and internal organs. Such changes are based on the following fact: The stimulation of receptors leads to the spread of the excitation to nearby structures of the spinal cord (more precisely to segments of the spinal cord). And these can be neurons responsible for the sweating of a specific area of the skin, regulate the temperature of the same area, ensure the activity of internal organs (heart, liver, intestines, etc. ), and maintain the tone of the muscles and blood vessels that are all these structuressupply. And when excitation is transferred to these neurons, there are corresponding symptoms of a violation of the activity of certain formations. Therefore, such a situation is quite possible if pain in the abdomen or in the area of the heart is caused by osteochondrosis of the thoracic spine.
Compression syndromes occur when the nerve root is compressed (stretched less often) as it leaves the intervertebral foramen, the tissues of the spinal cord, or the vessels that feed it. Compression syndromes are almost always caused by an existing herniated disc. The most common are hernias of the lower breast segments. Depending on the direction and location of the hernia, a person will experience certain symptoms. This can be represented as follows:
- Median (median) hernias are associated with the symmetrical development of muscle weakness in both legs and a loss of sensitivity in them. At the same time, the pain syndrome typical of compression of the nerve root is absent;
- lateral (lateral) hernias manifest exclusively pain associated with compression of the nerve root;
- mediolateral hernias combine the clinical symptoms of the previous two groups, only muscle weakness and sensory disorders predominate on the protruding disc side.
What kind of syndromes are considered in the context of osteochondrosis of the thoracic spine? Let's talk in more detail about the types of reflex and compression syndromes of this level.
Reflex Syndromes
Dorsago- sharp sudden pain in the thoracic spine. It is sharp in nature and is often described by patients as being struck with a dagger. Basically it can be felt between the shoulder blades, it can be given to the heart, the sternum. Patients are afraid to move and even to take deep breaths because it makes the pain worse (like shooting again). Very often these symptoms appear after a long stay in a steady, uncomfortable position during monotonous work. A sudden movement afterwards provokes dorsago in people with osteochondrosis of the thoracic spine. When palpating the thoracic spine, the tension of the paravertebral muscles appears in the form of a roller and its pain.
Sometimes such pain can be viewed as a heart attack, which appears so severe and sudden to the patient. However, the recorded electrocardiogram shows nothing abnormal, and the use of nitroglycerin under the tongue does not eliminate the pain.
Dorsalgiais another type of reflex chest syndrome. It is a pain syndrome that occurs gradually. The pain can be localized in any part of the back and chest. Painful pain, dull, sometimes with a touch of burning sensation (which is associated with irritation of the vegetative structures). It intensifies with movements of the spine, bending, turning on its own axis, coughing or sneezing, driving on an uneven road.
Pain can be felt along the intercostal spaces on one or both sides. This feature is due to the course of the nerve conductors (intercostal nerves and vessels are located in the intercostal space). In this case, by analogy with shingles, the pain is called intercostal neuralgia.
If the pain is localized on the anterior chest wall, it is also called pectalgia. However, it can only be felt in a few places with an intact back. For example, in the area of the xiphoid process or at the point of attachment of the sternocleidomastoid muscle. Very often, because of the pain and the dull nature of the pain, it is difficult to pinpoint exactly where it hurts: either something in the chest or in the superficial soft tissue area.
Dorsalgia can be accompanied by a reflex tension of the paravertebral muscles, which is more pronounced on the pain side. In this case, of course, muscle tension is not as pronounced as in a similar situation in the lumbar spine. However, muscle thickening is felt when palpated, and the touch itself causes discomfort or pain. Palpation of interspinous spaces and paravertebral points in the area of the segment affected by osteochondrosis is also painful.
Reflex syndromes in osteochondrosis of the thoracic spine are far more common than compression.
Compression syndromes
The compression of the nerve rootis mainly associated with a pain syndrome. The pain shoots in nature. The direction in which the pain spreads corresponds to the course of the nerve fibers. Thoracic osteochondrosis is an intercostal space. Because some of the nerve fibers form plexuses that are involved in innervation of internal organs, pain is felt in the chest and abdomen. The pain intensifies when moving, tilting the body, coughing, sneezing, laughing (because in these moments the tension of the root increases). In the zone where the compressed root is located, sensitivity disorders can be observed: crawling, numbness, tingling. Touching this area may not be well felt. In cases where the nerve root is subjected to compression for an extended period of time, movement disorders, that is, the weakness of the muscles it innervates, can occur. The muscles gradually atrophy. Movement disorders are very rare, however, as they are the youngest in the chronology of all symptoms. Usually, at the stage of pain and sensory disturbance, a person seeks medical help.
Spinal cord compressionmanifests itself in a weakness of the legs with a simultaneous increase in muscle tone (when the spinal cord in the lower thoracic spine is compressed, the muscle tone decreases). Pathological foot symptoms can occur (Babinsky and others). Sensitivity in the lower extremities is lost, the feeling of touching cold and hot is no different, the difference between just touching and an injection. Urinary tract diseases can occur with severe compression of the spinal cord.
The compression of blood vesselsthat supply the spinal cord leads to the development of myeloid ischemia, ie malnutrition of the spinal cord tissue. This, as well as compression of the spinal cord, is associated with the development of muscle weakness (patients say "legs have failed"), loss of sensation, and pelvic disorders.
One can rightly say that compression of the spinal cord and its vessels in osteochondrosis of the thoracic spine is very, very rare.
Vegetative components of osteochondrosis of the thoracic spine

Due to the fact that the nerve fibers coming from the thoracic spine contain autonomic conductors, irritation or injury to these fibers can be accompanied by autonomic symptoms. These can be:
- dryness and peeling of the skin in the area of innervation of a separate nerve;
- local violation of sweating and heat regulation (also according to the innervation zone);
- Chilliness of the lower extremities, brittle toenails;
- pain simulating gastrointestinal tract disorders (e. g. gastritis, peptic ulcer, cholecystitis, etc. );
- pain in the kidneys, which in fact has nothing to do with kidney pathology (there are no changes in urine and ultrasound);
- Pain in the heart area, very similar to angina pectoris and even myocardial infarction.
A characteristic of such pain can be the fact that a person may not experience back pain. This is initially misleading to both the patient and the medical staff when it comes to medical assistance. However, conducting a number of additional research methods makes it possible to exclude the pathology of the internal organs, and then osteochondrosis of the thoracic spine is considered the cause of such pain.
Treatment of osteochondrosis of the thoracic spine
All methods of treatment for osteochondrosis of the thoracic spine are divided into drugs and non-drugs. In most cases, only a combination of both groups will have an effect and the disease will regress. Although you need to understand that getting rid of thoracic spine osteochondrosis completely is simply impossible. The degenerative process can be suspended, slowed down, but does not develop in reverse.
Medicines
The main directions of drug exposure in osteochondrosis of the thoracic spine are the elimination of pain, the elimination of muscle tension, the improvement of microcirculation and tissue trophism.
Nonsteroidal anti-inflammatory drugs are successfully used to get rid of pain syndrome. Drugs in this group have the ability to reduce the inflammatory process, eliminate pain, and block platelet aggregation. The drugs are prescribed for an average of 7-14 days. This is usually enough to get rid of pain. Many of them are available in various forms (tablets, capsules, injection solutions, rectal suppositories), which makes them easy to use. In the first few days of treatment, drugs are used in injectable form and then switched to tablets or suppositories. The same drugs can be used locally at the same time: in the area of the thoracic spine. In addition, for this purpose there are also various forms of release: creams, ointments, gels, plasters.
Sometimes nonsteroidal anti-inflammatory drugs aren't enough to relieve pain. In such cases, you should resort to the use of analgesics. The mixtures are injected intravenously in saline or glucose.
Paravertebral blockade has a fairly good and quick analgesic effect. This is a type of medical manipulation when a medicinal substance is injected intracutaneously, subcutaneously, perineurally (right near the nerve or root) into the thickness of muscle tissue near the spine. The procedure requires certain skills and experience on the part of the doctor.
Local irritating and distracting ointments can also be used to relieve pain associated with osteochondrosis of the thoracic spine. These are ointments that contain snake venom, bee venom, and pepper extracts.
Muscle tension is relieved by non-drug methods.
Diuretics, hormones and escina lysinate are used to relieve edema of the nerve root.
Pentoxifylline, Dipyridamole, Complamin and Nicotinic Acid are used to normalize blood circulation, improve tissue nutrition and restore trophism.
With osteochondrosis of the thoracic spine, B vitamins are shown, which have analgesic and neurotrophic effects.
If the exacerbation of osteochondrosis of the thoracic spine has stopped, then you can resort to drugs that improve the metabolism of the intervertebral discs and joints. These are the so-called chondroprotectors. These drugs stimulate the regeneration of articular cartilage, interrupt the degenerative process in the intervertebral discs. They are prescribed for the long term (3-6 months).
Non-drug methods
These include:
- massage (classic, pointed, reflex-segmental);
- physical therapy exercises;
- stretching spasmodic muscles (there are special techniques, stretching is not "as you want");
- acupuncture;
- swimming (very useful for all patients with a localization of osteochondrosis);
- Physiotherapy (ultrasound, electrophoresis, amplipulse, diadynamic currents, mud therapy, etc. ).
If the hernia formed by osteochondrosis of the thoracic spine compresses the spinal cord, its vessels or nerve roots, and at the same time causes muscle weakness, dysfunction of the pelvic organs, pronounced pain syndrome (resistant to the use of drugs), then the question about conducting surgical treatment is considered.
Osteochondrosis of the thoracic spine is not a fatal disease, but it is very harmful to a sick person. It restricts his life, interferes with work and good rest. The main symptom of thoracic osteochondrosis is pain. It is impossible to get rid of this disease completely, but it is possible to suspend the degenerative process and minimize its manifestations.







































